Prospective Risk Adjustment
Clinically Relevant Insight into Patient Health
The CARAT risk adjustment suite surfaces medical conditions at the point of care to inform patient care and to improve revenue timing and accuracy.
A Complete Picture of the Data
Before you can accurately calculate a patient’s risk factor, you need to make sure you can both see and make sense of all the data in the patient record – regardless of how complex the notation or where the information resides.
CARAT gathers both structured and unstructured data from clinical notes, diagnostic tests, and claims in text, image or PDF format, leveraging optical character recognition (OCR), natural language processing (NLP), machine learning (ML), and algorithmic rules to surface everything you need to create an accurate picture of patient health. This entire process happens in real-time as an overlay within the EHR, providing insight right at the point of care.
AI-Powered Charting and Coding
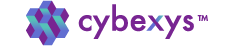
CARAT retrospective analysis helps surface conditions that need to be verified and coded by the provider or that require active M.E.A.T. management. CARAT ProviderAssist presents all actions as an overlay within the EHR, simplifying accurate and streamlined documentation.
CARAT analyzes clinical notes in the EHR concurrent to the encounter, helping to spot patterns and to suggest ICD-10 and HCC codes with higher accuracy. The CARAT AI continues to learn as you use it, integrating acronyms, phrasings, or misspellings to close the gap on automated coding.
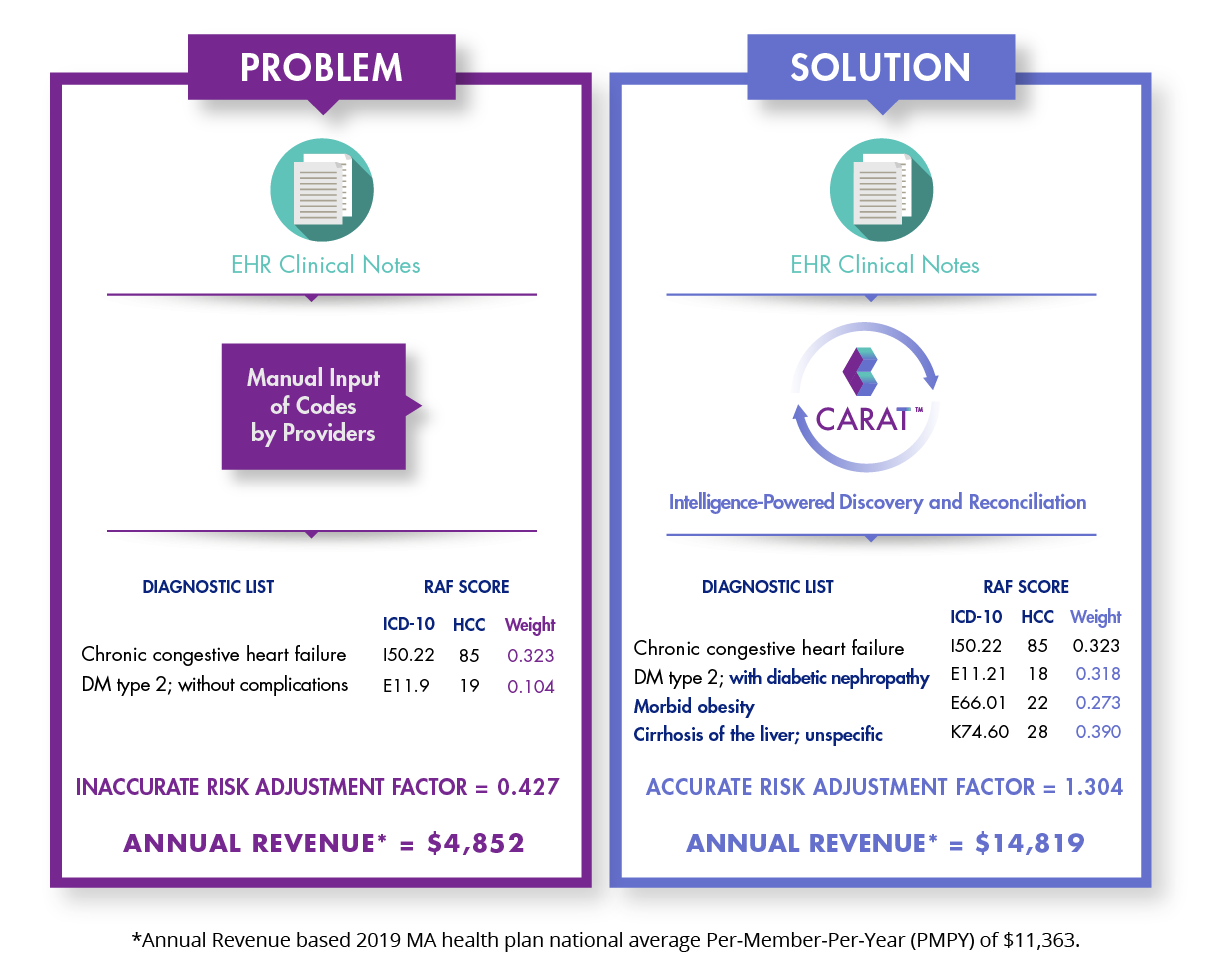
M.E.A.T. Validation
CARAT approaches every patient encounter with a retrospective analysis of clinical notes, diagnostic imaging, and specialist reports.
Either immediately after the encounter, or as a final check by a coder, CARAT validates M.E.A.T. criteria and highlights any CDI opportunities to meet CMS guidelines. The entire process takes just 5 minutes a day, simplifying a time-consuming process typically outsourced to coders.
The Power of CARAT
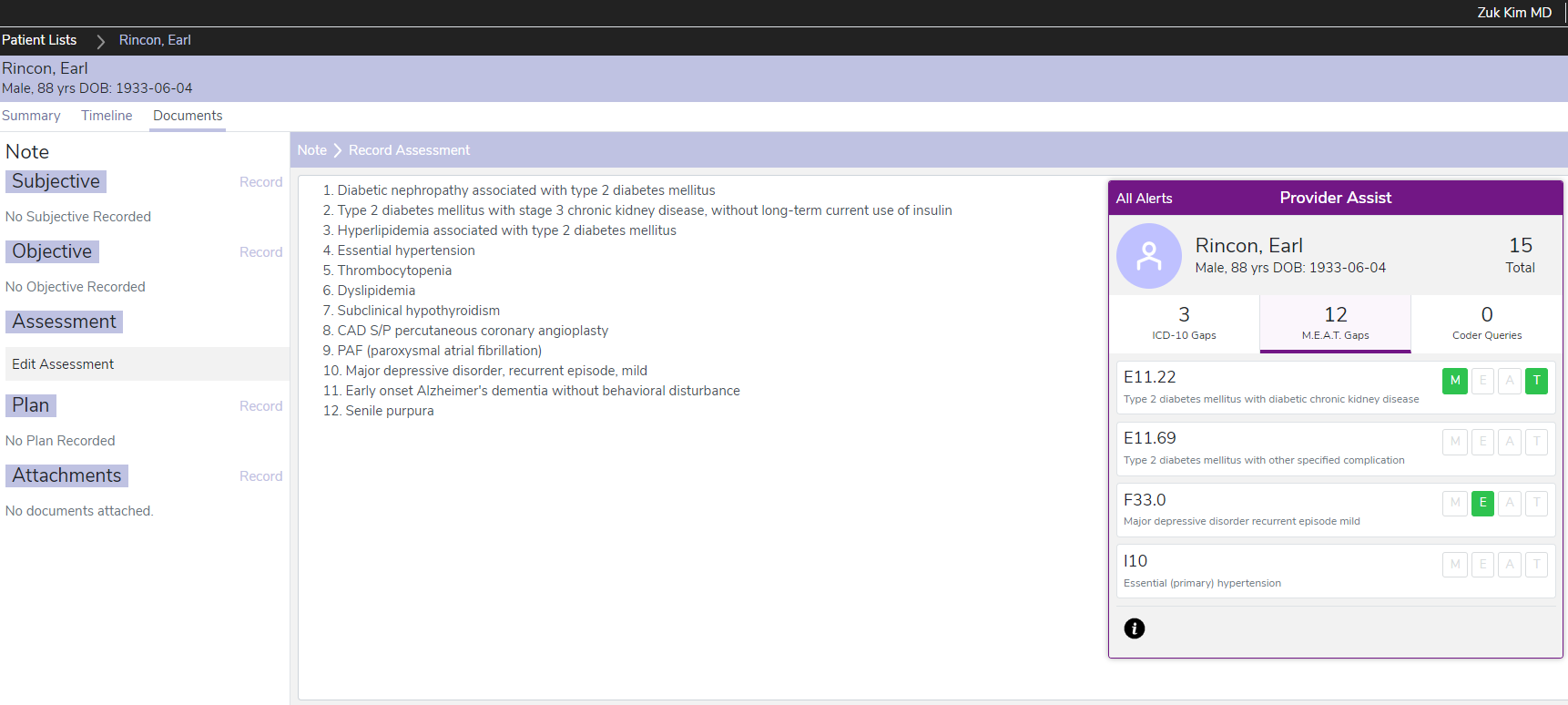
Cybexys findings involving numerous health plans and MCOs, hundreds of providers and thousands of patient encounters, CARAT has demonstrated the power to resolve under-coding and to lower risk exposure to RADV audits.
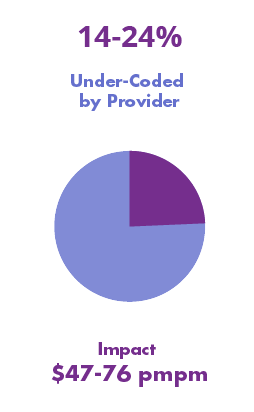
Under-documentation – Prior-years’ documented chronic conditions that were not included in the current year’s clinical notes.
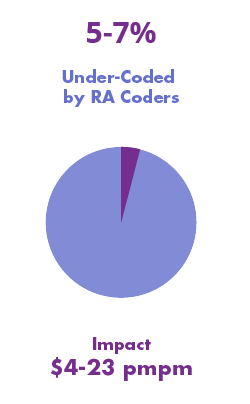
Under-scoring – the provider failed to assign proper ICD-10 codes to capture the severity of the diseases; however, the clinical notes support higher severity and complexity.
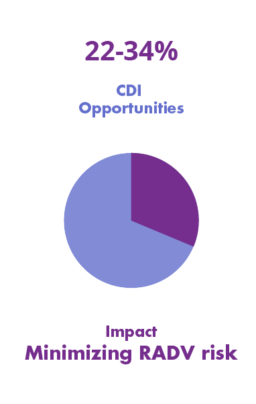
RADV Exposure / CDI Improvements – the provider missed proper documentation to support evidence of Monitoring, Evaluating, Assessing and Treating (M.E.A.T.) for the patient conditions included in the claims.