Health Plans
Risk Adjustment AI for Health Plans
The CARAT risk adjustment suite surfaces medical conditions within the EHR to inform patient care and to improve revenue timing and Prospective risk adjustment ensures providers approach every encounter with an accurate RAF and care continuity reflective of M.E.A.T. criteria accuracy.
Frictionless Transition to Prospective Risk Adjustment
CARAT gathers both structured and unstructured data from clinical notes, diagnostic tests, and claims in text, image or PDF format, leveraging optical character recognition (OCR), natural language processing (NLP), machine learning (ML), and algorithmic rules to surface everything you need to create an accurate picture of patient health. This entire process happens in real-time as an overlay within the EHR, providing insight right at the point of care.
Proven Capabilities
CARAT analyzes existing coding summary lists in the EHR, and/or claims submitted to the payer, plus the clinical notes created in the EHR from structured and unstructured data entry by clinicians (including PDFs).
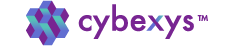
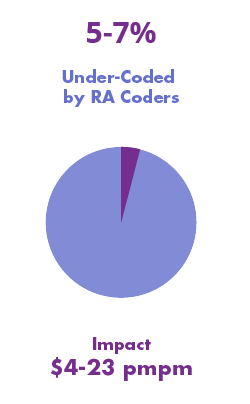
Cybexys findings involving numerous health plans and MCOs, hundreds of providers and thousands of patient encounters, CARAT has demonstrated the power to resolve under-coding and to lower risk exposure to RADV audits.
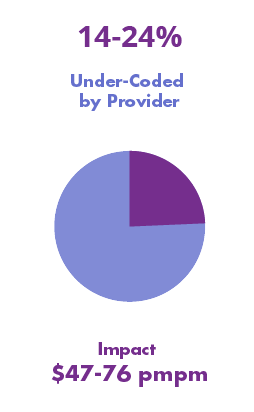
Under-documentation – Prior-years’ documented chronic conditions that were not included in the current year’s clinical notes.
Under-scoring – the provider failed to assign proper ICD-10 codes to capture the severity of the diseases; however, the clinical notes support higher severity and complexity.
RADV Exposure / CDI Improvements – the provider missed proper documentation to support evidence of Monitoring, Evaluating, Assessing and Treating (M.E.A.T.) for the patient conditions included in the claims.
CARAT ProviderAssist
CARAT ProviderAssist provides a concurrent review of clinical documentation during each encounter, presenting coding and documentation gaps in real-time from within the EHR. CARAT ProviderAssist identifies the severity of each patient condition and encouraging actions to inform their care and support clinical documentation consistent with [M]onitoring, [E]valuating, [A]ssessing, [T]reating criteria (M.E.A.T.) for each HCC code in the patient record.
CARAT completely eliminates the need for chase lists, allowing health plans to optimize for risk and quality at the provider level in real-time.
CARAT Analytics
CARAT Analytics is a cloud-based analytics portal that supports your population health management efforts to monitor risk scores and identify gaps between documentation and ICD-10 and HCC codes. CARAT Analytics helps you stratify your population, drill down to the provider level, and stay on top of trends and opportunities.
Coding or M.E.A.T. gaps are automatically presented to the provider as an overlay within the EHR with CARAT ProviderAssist, encouraging providers to take action to close gaps. Current and future encounters, supported by CARAT, encourage real-time validation of codes and M.E.A.T. criteria to eliminate chase lists.
CDI Opportunities
CARAT automates the review of previous years’ medical records to identify incomplete documentation in the current year’s notes, which may reflect missing continuity of medical care and compliance. By capturing newly inferred or chronic conditions, CARAT helps providers, utilization management, and care management teams support population health and value-based efforts.